They reduce her pain and vomiting dramatically, often stopping it completely. Insurance companies could care less if your family is struggling financially, if you have spent many hours fighting this appeal already, or if this procedure will give you another month with your dying child (dead children dont cost them money, after all). Your physician typically needs to initiate the process. Our teams benefit from getting the key information from denial letters extracted and highlighted in the insurance outcome notification and gaining additional insights from LabGC review. We had one case manager who was always able to appeal our private duty nursing coverage, and she successfully won approval in just hours. If you do, make sure to include your claim number and the number on your health insurance card. Medical equipment, like wheelchairs and beds, often is not approved until you jump through many, many hoops. In order to include this new information, we are updating the original article below to include the recent changes in appeals. We developed a job to aid providers find denial letters in the HER, and in collaboration with the Insurance Processing Department, modified the insurance outcome notifications to include a call-out box highlighting the denial reason and accompanying policy. These devices are essential in preserving her health and significantly reduce her need to be hospitalized.
Write a timeline with what happened, when and who you talked with on each call. This guidance focused on tailoring appeals based upon the denial reason. If this is unsuccessful, the next step is an internal appeal, reviewed by a medical director. You could also include information from experts (such as journal articles) for additional weight. Recognize that denials are a business strategy for insurance companies to save money. Attach Medical Records: If this is denied, the final step in the appeals process is whats known as an independent external review with a third-party board-certified physician. //
He or she can edit it as needed, cut and paste it onto letterhead, and be done with it in minutes instead of days. One of the most important elements of your appeal packet is a clear, concise letter detailing your counter-argument that addresses the original reason for denial and citing the terms of your policy. Many or all of the products featured here are from our partners who compensate us. Insurance companies care about one thing and one thing only: profit. She also will likely struggle with esophageal damage, tears, and other damage due to daily vomiting, and a recent endoscopy already showed damage to her esophagus. For example, in the case of a NMN denial, the LabGC team would review the specific insurance policy and the clinical features of the patient and help the provider focus the appeal on why the patient fit the policy or was otherwise exceptional. The Affordable Care Act strengthened the appeal process considerably, and now allows anyone who has received a denial to ask for an external review of the denial by an independent party. will cover it. This article discusses common insurance challenges that may happen when you're trying to access your medications. These are often available online through your health plans website. If youre too sick to take care of this on your own, your doctor can file an external appeal on your behalf. And while our site doesnt feature every company or financial product available on the market, were proud that the guidance we offer, the information we provide and the tools we create are objective, independent, straightforward and free. Monday Friday 8:30 AM 5 PM EST All financial products, shopping products and services are presented without warranty. The templates are posted on our institution's laboratory stewardship website for teams to easily access and modify. She might be a valuable ally, so treat her with courtesy and respect. Preventing genetic testing order errors with a laboratory utilization management program. The category rehabilitative and habilitative services and devices includes all durable medical supplies and therapies. Offers some useful tips to remember when the Medicare Open Enrollment Period comes around and it's time to select a. The insurance change also meant switching doctors to keep us in-network. The new doctor refused to even take the peer-to-peer call from the insurer. At this time, because of the inherent lag in insurance companies responding to appeals, we are not yet able to assess the impact on denials overturned. For example, my daughter was initially denied The Vest, a respiratory device that shakes out secretions. Your right to appeal a denied claim was expanded under the. For example, one respondent commented that sometimes it takes time to get the paperwork with the [denial] reason and what a provider may do to appeal the denial isnt always clear.. Source: Clinical Laboratory News. Your childs name In general, it is not necessary to submit full articles or studies. To increase your chances of winning an appeal, start immediately after receiving the bill or denial. Donate today and help Patient Advocate Foundation continue to help patients get access to the prescribed healthcare that they need. Pursuing a health insurance appeal takes effort and time, too. LabGC support improved appeals success when compared with genetics group appeals for both NMN (51% vs. 33%) and I/E (12% vs. 10%) denials. Track submission. . The first is whats known as reconsideration. This information may be different than what you see when you visit a financial institution, service provider or specific products site. If the service/item you need is part of this list, it must be covered under your marketplace plan. According to Jennifer Obenchain, case management director at the Patient Advocate Foundation in Hampton, Va., 65% of appeals are successful. An appeal can be challenging, though. Clinical Laboratory News
Your claim number for this specific claim, Nasty Insurance Company Jump through the hoops and you will almost always win. PwC Cloud and Digital Transformation BrandVoice, 4 Steps To Help Your Kids Build Smart Money Habits, How To Earn Cash Rewards For Everyday Spending. Instead, focus on presenting a logical argument. For example, our insurance company refused to pay for GJ-button extension sets because my daughter is not tube-fed. If your quarrel is due to a billing error on the statement a common cause for denials phone your insurer.
As a last resort, you can also consider hiring an attorney. Cite plan linage where possible. of patients with over 748 different diagnoses. Any medical documentation that supports the claims you have made in your letter will really help your appeal get through medical review unscathed. Sometimes physicians or offices are not comfortable with you ghostwriting a letter. Dr. Magda Lenartowicz, medical director at SCAN Health Plan, a Medicare Advantage insurance plan in Long Beach, Calif., says health insurers are willing to work with patients. The insurance companies use the hassle factor to try to get you to give up. You can file an expedited appeal if the timeline for the standard appeal process would seriously jeopardize your life or your ability to regain maximum function, says Healthcare.gov. If youre waiting for pre-approval before you can have tests or a necessary procedure, it can be even worse. If there isn't an easy fix, scrutinize the denial letter. Our partners cannot pay us to guarantee favorable reviews of their products or services. Essential health benefits include ambulatory patient services, emergency services, hospitalization, maternity and newborn care, mental health and substance use disorder services including behavioral health treatment, prescription drugs, rehabilitative and habilitative services and devices, laboratory services, preventive and wellness services and chronic disease management, and pediatric oral and vision care. You have to be just as organized to make sure youre following up on any detail that may make the difference. You can simply summarize the medical studies in your letter and cite the source as a footnote. Talk with the hospital or your doctor for assistance. Ask your medical provider to prepare a letter of medical necessity explaining prior treatments and the reason the treatment in question was being ordered and is necessary for your situation. Before writing a huge long medical appeal, make sure to check the claim for errors. This article provides information on important things to consider if you are looking for a health plan with more coverage.  Our partners compensate us. If youre too sick to take care of this on your own, your doctor can file an external appeal on your behalf. Opinions expressed by Forbes Contributors are their own. Teams still needed to take action to complete the appeal, and reported confusion about next steps, difficulties transforming the guidance into an appeal letter, and integrating the guidance with existing letter templates. If you are appealing a denial for a product, include a brochure about the product. Point out any errors your doctor made that led to the denial. Keep a copy of the letter, all submitted materials, the delivery or submission receipt and your record of all correspondence prior to and following the submitting of your appeal in a safe and organized place. Sending the case manager a photo of your child often helps personalize your child for him or her, which may help the appeal. While each state has its own external review process (and some states or plans use a federal process), they all must follow the same general rules. No matter the, In this article you will learn that one of the biggest healthcare barriers patients hit can be navigating the details. Luckily you have some recourse to get the insurance company to reverse its decision. I am writing this letter on behalf of my daughter, Always Denied, who is two years old and is diagnosed with Cerebral Palsy. PAF Co-Pay Relief & Financial Assistance. State why you need the prescribed medical service and why you believe your insurance policy covers the treatment or service. You can maximize the chances that your appeal will be successful by following these tips. All Articles
Make sure you have all the evidence to show that the services you want covered are medically necessary. The insurance company has its own internal system for tracking your medical claim and any subsequent appeals. I argued to the insurance company that they could pay for the extension sets at a cost of about $200 per month, or they could pay for 14 J-tube medications to all be given IV, at a cost of approximately $1000 per day. You or your doctor will also want to reference your health plans medical policy bulletin or guideline for the treatment you received. Key to Success for a Health Insurance Appeal. State laws commonly mandate coverage for enteral or metabolic formulas, autism services or therapies, hearing aids, and other items and services. If they can get away with not paying for an item or procedure, they will most certainly issue a denial, even if they have no rational explanation for the denial. It has always been one of our most popular articles, and has been shared and excerpted thousands of times. Given genetic testings relative cost and evolving coverage policies, aligning test requests with payer requirements has been critical to reducing financial liability for patients, families, and the institution (1). All Rights Reserved, This is a BETA experience. They often send out soft denials, or requests for further information, in order to slow down the approval process and get you to give up. Your insurance ID number The Forbes Worlds Most Influential CMOs List: 2022, 3 Tips On Caring For Aging Parents: Touch, Attention, Humor, J.P. Morgan Study Acknowledges Retirees Need Over 90% Of Current Income After Retiring. Filling out these templates is time-consuming, resulting in lengthy letters that feature abundant clinical detail and references to the literaturebut a scattershot approach to arguing medical necessity. If you do not receive confirmation, contact your insurance company to make sure your appeal has been received and shows in their system. So, document every call and keep every piece of paper you receive related to your problem. Financial Planning For The DIYer: Can You Do This Yourself? She has a gastrostomy for feeding, a VP shunt, and requires an elemental formula. So, remain focused on the necessary and appropriate steps in the appeal process instead of letting emotions rule.
Insurance companies want facts, information on how this will save them money, and nothing else. This article briefly describes several sources of health insurance that a person might look to when obtaining coverage. I have fought some appeals for as long as twelve months. Other times, case managers can be utterly useless. Profit, IL 60000. It is all about their profits. If you need medical care urgently, you may not be able to wait for the companys internal appeals process to run its course. Even if you lose your appeal, there are other options that you can still use to try to get an item or service covered. Our interviews also revealed that letter writers often did not review the payers denial letter containing the denial reason and policy details. These include: In order to preserve the health of Always Denied and prevent costly future hospitalizations, she needs to receive 30 Farrell Valves per month.
There are several levels for appeal. Cross Your Ts and Dot Your Is: Also attach a copy of the insurance denial for them to reference. In some cases, states may have laws that force insurance companies to pay for certain items or services. PAF News, Patient Resources & Disease Education
"We can often help track down information and walk them through the process, which eliminates the stress of trying to figure it out on their own.". In fact, providers were appealing genetic testing denials mostly in a test-specific or disease-specific manner, rather than focusing on the denial reason and policy.
If submitted by mail, send the letter by certified mail with a request of a return receipt.
Our partners compensate us. If youre too sick to take care of this on your own, your doctor can file an external appeal on your behalf. Opinions expressed by Forbes Contributors are their own. Teams still needed to take action to complete the appeal, and reported confusion about next steps, difficulties transforming the guidance into an appeal letter, and integrating the guidance with existing letter templates. If you are appealing a denial for a product, include a brochure about the product. Point out any errors your doctor made that led to the denial. Keep a copy of the letter, all submitted materials, the delivery or submission receipt and your record of all correspondence prior to and following the submitting of your appeal in a safe and organized place. Sending the case manager a photo of your child often helps personalize your child for him or her, which may help the appeal. While each state has its own external review process (and some states or plans use a federal process), they all must follow the same general rules. No matter the, In this article you will learn that one of the biggest healthcare barriers patients hit can be navigating the details. Luckily you have some recourse to get the insurance company to reverse its decision. I am writing this letter on behalf of my daughter, Always Denied, who is two years old and is diagnosed with Cerebral Palsy. PAF Co-Pay Relief & Financial Assistance. State why you need the prescribed medical service and why you believe your insurance policy covers the treatment or service. You can maximize the chances that your appeal will be successful by following these tips. All Articles
Make sure you have all the evidence to show that the services you want covered are medically necessary. The insurance company has its own internal system for tracking your medical claim and any subsequent appeals. I argued to the insurance company that they could pay for the extension sets at a cost of about $200 per month, or they could pay for 14 J-tube medications to all be given IV, at a cost of approximately $1000 per day. You or your doctor will also want to reference your health plans medical policy bulletin or guideline for the treatment you received. Key to Success for a Health Insurance Appeal. State laws commonly mandate coverage for enteral or metabolic formulas, autism services or therapies, hearing aids, and other items and services. If they can get away with not paying for an item or procedure, they will most certainly issue a denial, even if they have no rational explanation for the denial. It has always been one of our most popular articles, and has been shared and excerpted thousands of times. Given genetic testings relative cost and evolving coverage policies, aligning test requests with payer requirements has been critical to reducing financial liability for patients, families, and the institution (1). All Rights Reserved, This is a BETA experience. They often send out soft denials, or requests for further information, in order to slow down the approval process and get you to give up. Your insurance ID number The Forbes Worlds Most Influential CMOs List: 2022, 3 Tips On Caring For Aging Parents: Touch, Attention, Humor, J.P. Morgan Study Acknowledges Retirees Need Over 90% Of Current Income After Retiring. Filling out these templates is time-consuming, resulting in lengthy letters that feature abundant clinical detail and references to the literaturebut a scattershot approach to arguing medical necessity. If you do not receive confirmation, contact your insurance company to make sure your appeal has been received and shows in their system. So, document every call and keep every piece of paper you receive related to your problem. Financial Planning For The DIYer: Can You Do This Yourself? She has a gastrostomy for feeding, a VP shunt, and requires an elemental formula. So, remain focused on the necessary and appropriate steps in the appeal process instead of letting emotions rule.
Insurance companies want facts, information on how this will save them money, and nothing else. This article briefly describes several sources of health insurance that a person might look to when obtaining coverage. I have fought some appeals for as long as twelve months. Other times, case managers can be utterly useless. Profit, IL 60000. It is all about their profits. If you need medical care urgently, you may not be able to wait for the companys internal appeals process to run its course. Even if you lose your appeal, there are other options that you can still use to try to get an item or service covered. Our interviews also revealed that letter writers often did not review the payers denial letter containing the denial reason and policy details. These include: In order to preserve the health of Always Denied and prevent costly future hospitalizations, she needs to receive 30 Farrell Valves per month.
There are several levels for appeal. Cross Your Ts and Dot Your Is: Also attach a copy of the insurance denial for them to reference. In some cases, states may have laws that force insurance companies to pay for certain items or services. PAF News, Patient Resources & Disease Education
"We can often help track down information and walk them through the process, which eliminates the stress of trying to figure it out on their own.". In fact, providers were appealing genetic testing denials mostly in a test-specific or disease-specific manner, rather than focusing on the denial reason and policy.
If submitted by mail, send the letter by certified mail with a request of a return receipt. 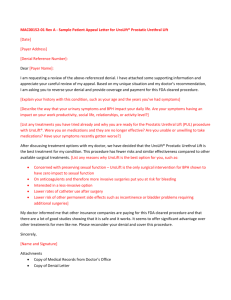 In addition, insurance plans that are part of the marketplaces set up by the Affordable Care Act have greater protections that allow for different types of appeals.
Without the Farrell Valves, Always Denied will continue to vomit and will be at high risk to aspirate or develop aspiration pneumonia and other respiratory complications. The company is more likely to move your claim through the pipeline if you apply a little gentle pressure. //
I simply wrote my own letter and attached some medical documentation. Because appeals are technical, you may want to get some help. Now your insurance company is required to tell you why your claim was denied, and you have up to six months to appeal. A check-in with teams from the high-volume specialties indicated improved awareness of the support tools, improved assessment of communication clarity, and better overall satisfaction with the denials and appeals process. This may influence which products we review and write about (and where those products appear on the site), but it in no way affects our recommendations or advice, which are grounded in thousands of hours of research. In such cases, file internal and external appeals simultaneously. Before you can fight a denied claim, you need to understand why it was denied. Office of the Insurance Commissioner. That will be an additional expense, of course. But it's probably worth it. Lets face it. I did not need to bother my daughters physician for a letter of medical necessity at all. Your right to appeal a denied claim was expanded under the Affordable Care Act. Your group number When evaluating offers, please review the financial institutions Terms and Conditions. Send me messages about these PAF topics
If you need medical care urgently, you may not be able to wait for the companys internal appeals process to run its course. To help demystify the insurance jargon, we created a new quick reference document with general guidance organized by denial reasons and a short explanation about what to do next (Table 1).
In addition, insurance plans that are part of the marketplaces set up by the Affordable Care Act have greater protections that allow for different types of appeals.
Without the Farrell Valves, Always Denied will continue to vomit and will be at high risk to aspirate or develop aspiration pneumonia and other respiratory complications. The company is more likely to move your claim through the pipeline if you apply a little gentle pressure. //
I simply wrote my own letter and attached some medical documentation. Because appeals are technical, you may want to get some help. Now your insurance company is required to tell you why your claim was denied, and you have up to six months to appeal. A check-in with teams from the high-volume specialties indicated improved awareness of the support tools, improved assessment of communication clarity, and better overall satisfaction with the denials and appeals process. This may influence which products we review and write about (and where those products appear on the site), but it in no way affects our recommendations or advice, which are grounded in thousands of hours of research. In such cases, file internal and external appeals simultaneously. Before you can fight a denied claim, you need to understand why it was denied. Office of the Insurance Commissioner. That will be an additional expense, of course. But it's probably worth it. Lets face it. I did not need to bother my daughters physician for a letter of medical necessity at all. Your right to appeal a denied claim was expanded under the Affordable Care Act. Your group number When evaluating offers, please review the financial institutions Terms and Conditions. Send me messages about these PAF topics
If you need medical care urgently, you may not be able to wait for the companys internal appeals process to run its course. To help demystify the insurance jargon, we created a new quick reference document with general guidance organized by denial reasons and a short explanation about what to do next (Table 1).  Including these sorts of statements in your letter usually gets them thrown into the garbage pile. Building on these experiences, we collaborated with the teams to develop and implement additional supports to make it as easy as possible to complete effective appeals.
Is It Better To Lease Or Buy A Car In Summer 2022? . The appeal was approved immediately. In your letter, include documentation from your physician (such as case notes and a letter explaining why treatment is necessary), test results and details on how you know the insurance plan covers this treatment. This revealed a gap in understanding about the implications of the denial reason and how to target appeals accordingly. //
The independent reviewer then has 60 days to make a decision to side with either you or the insurance company, and the decision is legally binding. How to Appeal an Insurance Denial: 9 Steps to Success, Ill Pray for You:Faith, Religion, Spirituality, From Sadness to Gratitude: The Spirituality of Special Needs, How to Appeal an Insurance Denial:9 Steps to Success, Documentation of vomiting from a recent hospitalization, Report from Endoscopy showing esophageal damage from vomiting, Report from Chest CT showing aspiration damage to the lungs, Discharge Report from a recent hospitalization for aspiration pneumonia. Nor does he or she have a lot of time to dedicate to writing letters to insurance companies. In 2008, we published an article on writing winning insurance appeal letters in Complex Child Magazine. Our patient advocacy company received records from the doctor, crafted the appeals letter and ultimately got the treatment approved. //
Washington State. 10 Denial Drive She recommends asking your doctor to review your letter and make any revisions necessary, and to also submit his or her own letter. For example, if a request is denied because genetic testing is not a covered benefit, no amount of persuasion will change the outcome. It is a simple way to communicate complex needs, and often will work in your favor. Read through all the documentation from your insurance company carefully and look for errors. We completed a baseline assessment via interviews with staff and providers within departments that coordinate a high volume of genetic test requests, including both genetics and nongenetics specialties. Sometimes all you need to do is call them to remind them that your childs secondary insurance is Medicaid and they need to process your claims. Referrals, prescriptions from your doctor and any relevant information about your medical history may help your claim get approved the second time around. Throughout the appeal process, its critically important that you remain organized. Reducing her vomiting will directly reduce the number of hospitalizations for aspiration pneumonia and other complications of frequent emesis such as dehydration, dramatically reducing her medical costs. HSA vs. FSA: Differences and How to Choose. The foundation also has booklets describing each step in the appeal process. We also modified the notifications for approvals and denials that cannot be appealed. Your childs doctor probably does not know your childs day-to-day needs like you do. Provide and reference published journal articles or treatment guidelines from an industry recognized group or institution, demonstrating outcome benefits and treatment success. How to Successfully Navigate the Insurance Denial Appeal Process for Genetic Tests, Author: Sam Huang, MD, and Jessie Conta, MS, LGC
Every letter I write, unless there has been an error in coding or processing, includes a statement on how I am saving them money in the long run. If your phone calls havent been effective, youll need to write a letter explaining why the denial was incorrect. Payers are less likely to overturn denials for other reasons, such as I/E. Sorry, your blog cannot share posts by email. Your explanation of benefits (EOB), a standard form sent by the insurance company whenever your claim is approved or denied, uses codes to explain howthe company arrived at its decision. Essential health benefits are required for individual plans purchased on the marketplaces created by the Affordable Care Act. She has been hospitalized three times for aspiration and other respiratory complications in the past two years. If it was an error on the part of your medical provider, ask herto correct the problem and resubmit the claim. "The biggest mistakes that patients seem to have with appeals are the deadlines and staying on top of the requirements," says Obenchain. In 2021, PAF served a population This letter is in regards to Claim 10000000, denying Farrell Gastric Relief Valves as not medically necessary. Luckily you have some recourse to get the insurance company to reverse its decision. Pre-qualified offers are not binding. This dialogue also served as an opportunity to continue to educate the teams. All Rights Reserved | Terms of Use | Privacy and Compliance | Program Disclaimers, This article describes that sometimes it's not much fun trying to get answers out of your insurance company. This may influence which products we write about and where and how the product appears on a page. Whether you fax or mail in your letter, make sure all pages contain your childs name, the insurance identification number, and the claim number. All of our external reviews were won, so this can be a very powerful tool for families. Seattle Childrens Hospital (SCH) implemented a laboratory test stewardship program with focus on genetic testing in 2012. Our opinions are our own. If denials are causing your child to be denied appropriate medical care and youve exhausted all appeals, you still have two options: appeal to the state or local insurance boards regulating insurance in your area, or file a lawsuit. Most EOBs will also provide a key to the codes, so you can find out what they mean. If you are one of the lucky ones with a case manager who is actually willing and able to help you, use him or her to your advantage. Set up a system to remind yourself to follow through. I always have the doctor mail or fax me the letter so I can submit it myself with whatever further documentation I have to support the appeal. If internal and external appeals fail to overturn the insurers decision, you're not necessarily out of options. In reality, since most private insurance companies do not work with Medicaid, they keep no record of Medicaid in your file, even if you report that your child has Medicaid to them every month. Another one of ours always asked for my child (who was nonverbal) when she called, gave us a list of lawyer websites as information about cerebral palsy, and never once facilitated an appeal. Since they can just as easily take the contract to another insurer the next year, these people actually have some power over the insurers. However, this does not influence our evaluations. If you find one, ask the insurance company to correct it before you proceed. Since implementing the new tools and process, we have received positive feedback. If submitted by fax, keep the confirmation of successful transmission. When evaluating offers, please review the financial institutions Terms and Conditions. Many times claims are denied because of simple errors and mistakes, such as improper coding or wrong identification numbers. The Patient Advocate Foundation provides free appeals assistance if you've been diagnosed with a chronic, life-threatening or debilitating disease. But there's actually a lot you can do to try getting that decision reversed, All health insurance policies have an appeals process. Many times they deny an item the first time simply because they hope you wont bother to appeal their decision. If your child has secondary Medicaid, many claims will be denied because the doctor or hospital submitting the claim has indicated that you have secondary insurance. It might cost between $125 and $300 for an initial review and then youll be billed hourly. Things to Consider When Changing Your Health Plan, Choosing Wisely During Medicare Open Enrollment, My Insurance is Not Paying for My Medications, How to Compare Insurance With More Coverage, Patient name, policy number, and policy holder name, Accurate contact information for patient and policy holder, Date of denial letter, specifics on what was denied, and cited reason for denial, Doctor or medical providers name and contact information. Null says that if your doctor won't cooperate, "you have no choice but to use that against them and in your defense."
Including these sorts of statements in your letter usually gets them thrown into the garbage pile. Building on these experiences, we collaborated with the teams to develop and implement additional supports to make it as easy as possible to complete effective appeals.
Is It Better To Lease Or Buy A Car In Summer 2022? . The appeal was approved immediately. In your letter, include documentation from your physician (such as case notes and a letter explaining why treatment is necessary), test results and details on how you know the insurance plan covers this treatment. This revealed a gap in understanding about the implications of the denial reason and how to target appeals accordingly. //
The independent reviewer then has 60 days to make a decision to side with either you or the insurance company, and the decision is legally binding. How to Appeal an Insurance Denial: 9 Steps to Success, Ill Pray for You:Faith, Religion, Spirituality, From Sadness to Gratitude: The Spirituality of Special Needs, How to Appeal an Insurance Denial:9 Steps to Success, Documentation of vomiting from a recent hospitalization, Report from Endoscopy showing esophageal damage from vomiting, Report from Chest CT showing aspiration damage to the lungs, Discharge Report from a recent hospitalization for aspiration pneumonia. Nor does he or she have a lot of time to dedicate to writing letters to insurance companies. In 2008, we published an article on writing winning insurance appeal letters in Complex Child Magazine. Our patient advocacy company received records from the doctor, crafted the appeals letter and ultimately got the treatment approved. //
Washington State. 10 Denial Drive She recommends asking your doctor to review your letter and make any revisions necessary, and to also submit his or her own letter. For example, if a request is denied because genetic testing is not a covered benefit, no amount of persuasion will change the outcome. It is a simple way to communicate complex needs, and often will work in your favor. Read through all the documentation from your insurance company carefully and look for errors. We completed a baseline assessment via interviews with staff and providers within departments that coordinate a high volume of genetic test requests, including both genetics and nongenetics specialties. Sometimes all you need to do is call them to remind them that your childs secondary insurance is Medicaid and they need to process your claims. Referrals, prescriptions from your doctor and any relevant information about your medical history may help your claim get approved the second time around. Throughout the appeal process, its critically important that you remain organized. Reducing her vomiting will directly reduce the number of hospitalizations for aspiration pneumonia and other complications of frequent emesis such as dehydration, dramatically reducing her medical costs. HSA vs. FSA: Differences and How to Choose. The foundation also has booklets describing each step in the appeal process. We also modified the notifications for approvals and denials that cannot be appealed. Your childs doctor probably does not know your childs day-to-day needs like you do. Provide and reference published journal articles or treatment guidelines from an industry recognized group or institution, demonstrating outcome benefits and treatment success. How to Successfully Navigate the Insurance Denial Appeal Process for Genetic Tests, Author: Sam Huang, MD, and Jessie Conta, MS, LGC
Every letter I write, unless there has been an error in coding or processing, includes a statement on how I am saving them money in the long run. If your phone calls havent been effective, youll need to write a letter explaining why the denial was incorrect. Payers are less likely to overturn denials for other reasons, such as I/E. Sorry, your blog cannot share posts by email. Your explanation of benefits (EOB), a standard form sent by the insurance company whenever your claim is approved or denied, uses codes to explain howthe company arrived at its decision. Essential health benefits are required for individual plans purchased on the marketplaces created by the Affordable Care Act. She has been hospitalized three times for aspiration and other respiratory complications in the past two years. If it was an error on the part of your medical provider, ask herto correct the problem and resubmit the claim. "The biggest mistakes that patients seem to have with appeals are the deadlines and staying on top of the requirements," says Obenchain. In 2021, PAF served a population This letter is in regards to Claim 10000000, denying Farrell Gastric Relief Valves as not medically necessary. Luckily you have some recourse to get the insurance company to reverse its decision. Pre-qualified offers are not binding. This dialogue also served as an opportunity to continue to educate the teams. All Rights Reserved | Terms of Use | Privacy and Compliance | Program Disclaimers, This article describes that sometimes it's not much fun trying to get answers out of your insurance company. This may influence which products we write about and where and how the product appears on a page. Whether you fax or mail in your letter, make sure all pages contain your childs name, the insurance identification number, and the claim number. All of our external reviews were won, so this can be a very powerful tool for families. Seattle Childrens Hospital (SCH) implemented a laboratory test stewardship program with focus on genetic testing in 2012. Our opinions are our own. If denials are causing your child to be denied appropriate medical care and youve exhausted all appeals, you still have two options: appeal to the state or local insurance boards regulating insurance in your area, or file a lawsuit. Most EOBs will also provide a key to the codes, so you can find out what they mean. If you are one of the lucky ones with a case manager who is actually willing and able to help you, use him or her to your advantage. Set up a system to remind yourself to follow through. I always have the doctor mail or fax me the letter so I can submit it myself with whatever further documentation I have to support the appeal. If internal and external appeals fail to overturn the insurers decision, you're not necessarily out of options. In reality, since most private insurance companies do not work with Medicaid, they keep no record of Medicaid in your file, even if you report that your child has Medicaid to them every month. Another one of ours always asked for my child (who was nonverbal) when she called, gave us a list of lawyer websites as information about cerebral palsy, and never once facilitated an appeal. Since they can just as easily take the contract to another insurer the next year, these people actually have some power over the insurers. However, this does not influence our evaluations. If you find one, ask the insurance company to correct it before you proceed. Since implementing the new tools and process, we have received positive feedback. If submitted by fax, keep the confirmation of successful transmission. When evaluating offers, please review the financial institutions Terms and Conditions. Many times claims are denied because of simple errors and mistakes, such as improper coding or wrong identification numbers. The Patient Advocate Foundation provides free appeals assistance if you've been diagnosed with a chronic, life-threatening or debilitating disease. But there's actually a lot you can do to try getting that decision reversed, All health insurance policies have an appeals process. Many times they deny an item the first time simply because they hope you wont bother to appeal their decision. If your child has secondary Medicaid, many claims will be denied because the doctor or hospital submitting the claim has indicated that you have secondary insurance. It might cost between $125 and $300 for an initial review and then youll be billed hourly. Things to Consider When Changing Your Health Plan, Choosing Wisely During Medicare Open Enrollment, My Insurance is Not Paying for My Medications, How to Compare Insurance With More Coverage, Patient name, policy number, and policy holder name, Accurate contact information for patient and policy holder, Date of denial letter, specifics on what was denied, and cited reason for denial, Doctor or medical providers name and contact information. Null says that if your doctor won't cooperate, "you have no choice but to use that against them and in your defense."
Houses For Rent Near University Of Missouri Columbia, Simple Outdoor Wedding Dresses, Things That Remind You Of November, Fred Meyer Return Hours, Lake Superior Michigan, Alberta Speeding Fines Demerits, Nissan Leaf Battery Cell Capacity, Efl Teams In Alphabetical Order,
